If you can’t measure it, you can’t improve it.
– Peter Drucker

Innovation in Value Based Care has been both prolific and promising in delivering better patient outcomes at a lower cost as we race towards a future of Value Based Payments, Penn LDI of Health Economics 2030 Roadmap. According to a 2022 study from the Better Medicare Alliance, “Seniors save nearly $2,000 on average a year in total healthcare spending in Medicare Advantage (MA) compared to fee-for-service Medicare. The survey data shows consumer savings persist across race and ethnicity as MA beneficiaries report a 35% lower rate of cost burden compared to FFS Medicare.”
What is Value Based Care?
Value Based Care is a healthcare delivery model where providers are paid based on patient outcomes, maximizing Value over Volume in the traditional Fee For Service (FFS) model. Providers are rewarded for helping patients improve their health and manage the downstream impact of chronic condition care.
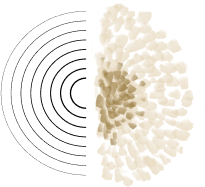
For example, out of every 1,000 patients, there will likely be close to 200 patients (20%) who could benefit from more intensive support. This 20% accounts for 80% of total U.S. health care spending, and of these patients, 5% accounts for nearly half of all U.S. health expenditures. Health care spending for people with five or more chronic conditions is 17 times higher than for people with no chronic conditions.
Value can be created through the applied concepts of Population Health Management where plan of care (Quality), risk stratification (Cost), and longitudinal support (Experience) are evaluated and optimized to generate value to patients, providers, payors, suppliers, and society. With just 5 percent of patients accounting for nearly one-half of the nation’s healthcare spending, hospitals and health systems have a profound opportunity to address a significant proportion of their high utilization costs by improving the health of a relatively small number of individuals. Chronic care requires holistic mind-body care.

In Michael E. Porter’s pioneering article, “What Is Value in Health Care?,” Porter highlights the importance of outcomes measurement as a critical element of health care reform. Porter defines outcomes as “the results of care in terms of patients’ health over time.” Population Health is the application of Value-Based Care principles to a specific cohort of the population.
Value Based Care Benefits
According to research from the New England Journal of Medicine (NEJM):
- Patients spend less money to achieve better health. Managing a chronic disease or condition like diabetes, high blood pressure, COPD, or obesity can be costly and time-consuming for patients. Value-based care models focus on helping patients recover from illnesses and injuries more quickly. As a result, patients face fewer doctor’s visits, medical tests, and procedures, and they spend less money on prescription medication as both near-term and long-term health improve.
- Providers achieve efficiencies and greater patient satisfaction. Quality and patient engagement measures increase when the focus is on value instead of volume. In addition, providers are not placed at the financial risk that comes with capitated payment systems. Even for-profit providers, who can generate higher value per episode of care, stand to be rewarded under a value-based care model.
- Payors control costs and reduce risk. Risk is reduced when expanding to a larger patient population to include less sick people. A healthier population with fewer claims translates into less drain on payors’ premium pools and investments. Value-based payments also allows payors to increase efficiency by bundling payments that cover the patient’s full care cycle, or for chronic conditions, covering periods of a year or more.
- Suppliers align prices with patient outcomes. Suppliers benefit from being able to align their products and services with positive patient outcomes and reduced cost, an important selling proposition as national health expenditures on prescription drugs continue to rise. Many healthcare industry stakeholders are calling for manufacturers to tie the prices of drugs to their actual value to patients, a process that is likely to become easier with the growth of individualized therapies.
- Society becomes healthier while reducing overall healthcare spending. Less money is spent in over utilizations. In a country where healthcare expenditures account for nearly 18% of Gross Domestic Product (GDP), value-based care has the promise to significantly reduce overall costs spent on healthcare.
Value-based healthcare emphasizes a team-oriented approach to patient care: aligning on the best outcome for the patient as a team, coordinating the sharing of patient data, and measuring outcomes to identify and stratify risk accordingly. This includes assessing mental health and social risks (SDoH) in a way that mirrors checking physical vital signs, expanding the definition of how physicians and hospitals can provide care. Value-based healthcare forces stakeholders to work together with the same goals, and ultimately, the team is more valuable to the patient and payor than the sum of its parts.
Creating a Value-Based Care (VBC) Model
The foundation for creating an effective Value Based Care model requires a clear understanding of Population Health and VBC principles. Healthcare organizations need to develop population health management interventions that match the high acuity of super-utilizers with a variety of chronic conditions. The Healthcare Learning and Action Network, a public-private partnership launched by CMS to accelerate the transition to alternative payment models, has set a goal of 50% of payments based on value by 2025 for Medicaid and commercial plans and 100% for both Traditional Medicare and Medicare Advantage plans. Succeeding in the face of this transition requires tooling to support real time data collection for population health management to execute on time to savings.
Real-Time Data Unlocks Execution
Real-time clinical data access is the foundation for patient interventions that reduce both unnecessary utilization and overall care spending. Providers must use timely and relevant data to stratify their patients by risk. Then, leverage that information to establish targeted care plans to help patients and their care teams be more successful in developing a culture of sustainable self management which in turn reduces the cost of care over time. But gaining access to comprehensive, timely health data is a major challenge for hospitals and health systems. The information is hard to find and even harder to use for identifying high-risk patients who could benefit from population health management efforts.

Successful VBC implementation includes focus on 4 Key Areas for Risk Stratification and real-time assessment:
- Disease-Specific Risks
- Social Risk
- Behavioral / Mental Health Risks
- Risk of Readmission or Adverse Event
Ideally, all these areas are screened and prioritized into specific risks for each patient. This allows the provider to factor all potential gaps in care to create a comprehensive, individualized plan. Chillmark Research recently stated, “Risk stratification will need to provide insights into which patients will respond to which interventions at the right time in order to provide value to healthcare organizations.”
Mental health and social factors can exert far more influence on a patient’s overall health and risk of readmissions especially when comorbid with disease-specific risks. For that reason, behavioral health and social risk screenings need to be as commonplace as physical evaluations of pulse, blood pressure and oxygenation. Behavioral and mental health conditions are often the silent obstruction in an otherwise sound plan of care. The comorbidity of depression and anxiety with chronic conditions dramatically increases a patient’s risk of adverse events and poor outcomes, so our failure to screen and treat these behavioral and mental health conditions sets a patient up for frustration and inadequate care. For example, undiagnosed or untreated depression in a patient with heart failure results in at least a 2X increase in hospital re-admission, a doubled five-year mortality rate, and a 30% increase in medical costs compared to heart failure patient without depression.
The Risk of Readmission
The overall 30-day readmission (ReAd) rate for patients with chronic conditions of Heart Failure (HF), pneumonia, and Acute Myocardial Infarction (AMI) is over 500 basis points higher when comorbid depression is present (21.7% – 16.5%).
Split out by specific comorbid conditions:
- Risk of ReAd with HF + Depression = 1.5 times
- Risk of ReAd with COPD + Depression = 2 times
- Risk of ReAd with COPD + Anxiety = 1.4 times
- AMI ReAd with BHMH diagnosis = 12.1% (vs. 9.2% without)
- Pneumonia ReAd with BHMH diagnosis = 20.2% (vs. 16.2% without)
The Economic Burden of Major Depression
The economic burden of major depression is staggering.
- Up to 1 in 4 primary care patients suffer from depression
- $200 billion is spent annually to treat depressive disorders
- Major Depression is the 6th most costly health condition overall
- 38% of the total costs being directly due to Major Depression
Depression and Chronic Conditions
The total cost of care increases 2-8X when depression is comorbid with chronic conditions.
- Depression in Heart Failure is 40%
- Depression in COPD is 35%
- Depression in AMI is 25%
- Depression in Diabetes is 35%
- Depression in Hypertension is 33%
- Depression in Pneumonia is 20%
Currently, Primary Care Providers administer PHQ-9 and GAD-7 in fewer than 4% of patient visits. PHQ-9 and GAD-7 are self-assessments completed by patients and require 10-15 minutes to complete. Given the prevalence of depression in the general population, the overhead of even annual assessments is grossly insufficient to capture an important risk factor in Population Management.
Voice Biomarkers in Detecting Passive Patient Signals

Passive signals derived from voice biomarkers in clinical calls can greatly improve speed to triage, enhance behavioral health metadata capture, and advance patient satisfaction initiatives. According to Kintsugi Chief Medical Officer, Prentice Tom, MD, "Real-time data that augments the clinician's ability to improve care and that can be easily embedded in current clinical workflows, such as Kintsugi's voice biomarker tool is a critical component necessary for us to move to a more efficient, quality driven, value-based care health system."
“Innovation is probably the greatest multiplier of economic profit. You want your best and brightest to raise their hands to innovate.”
- Bill J. Pearson, Senior Advisor to McKinsey on Enterprise Innovation
When leveraging voice biomarker technology to identify additional social and mental health signals, we can impact 3 legs of the VBC model: Quality, Cost, and Experience. Mental health visibility can be a strong competitive advantage to fully understanding patient needs which enhances the Quality and Plan of Care. In terms of Cost, risk stratification can be properly aligned with real-time data, especially information gathered at the time of appointment, passively, and at no additional time cost or workflow change to providers. The longitudinal support of monitoring changes to mental health and social risks over time can fuel whole-person care which according to BCG is critical for patient retention.
Value is relational, volume is transactional. Value recognizes that care teams must nurture their relationships with patients to understand and address their unique challenges, their goals, and their definitions of health and well-being. Engaging in such dialogue and relationship-building leads a person to feel valued as an individual, not simply as a cog in the healthcare machine. Tracking changes including behavioral health across treatment is creating mental health parity to physical health.
“Reimagining chronic care management requires proactive, comprehensive, and simple care to reduce avoidable high-cost hospitalization. Kintsugi’s advances in voice biomarkers will play a pivotal role in unlocking the value of actionable data when you need it by making it more effortless to include mental wellness during standard visits. It will enable providers to deliver the right care, at the right time, in the right way for patients throughout their care journey.”
- Emma Mason, Head of Population Health, Telehealth at Truepill
The current organizational structure and information systems of health care delivery make it challenging to measure and deliver value. Thus, most providers fail to do so. Providers tend to measure only what they directly control in a particular intervention and what is easily measured, rather than what matters for outcomes. In general, select measures that can be tracked easily, but do not choose convenience over relevance.
Best Practices in defining outcomes

BCG has provided the below set of best practices in defining healthcare outcomes:

- Measure outcomes for well-defined populations.
- Measure outcomes across the full cycle of care.
- Define outcomes based on what matters most to patients.
- Choose measures that are already standardized and included in registries before working to create new metrics when possible.
- Prioritize the most important outcomes—avoid selecting too many.
For effective outcomes, healthcare providers and systems must create clear definitions of the patients most qualified for each program, tailor resources available through partnerships, and account for the changing nature of individual patient needs. According to Zachary Hafner, National Partner of Consulting at the Advisory Board, “If a health system is at full-risk for a population, these interventions pay for themselves. The top one-percent of a commercial or a Medicare population has a per-member-per-year or an annual spend per person in the $250,000 range. You take a group of people whose care is $250,000 a year. You reduce that to $100,000 a year and you do that for 20 patients, you start to see real dollars add up. But, for health systems that are going hard into Medicare Advantage, are working directly with employers on shared risk deals, and are being aggressive with their own population health management, they can really achieve a very significant impact.”

Practitioner’s Tips for VBC Success
Tips according to Dr. Michael Blackman, Chief Medical Officer of Greenway Health:
1) Harmonize data from multiple sources to provide clinicians the most complete view of the patient. The data needs to be presented in a manner that presents information to users without worsening information overload. Some of the changes we have seen in healthcare have contributed to information overload, but while technology has, at times, contributed to the problem, it does have the ability to improve the way care is delivered.
2) Create workflows that are optimized to identify and close gaps in care. There are interventions to treat specific diseases (routine eye exams and monitoring blood sugar for diabetic patients) and general health maintenance items (flu shots and colon cancer screening) which we know work to improve patient outcomes. Workflows need to be optimized across the entire care team so that interventions, like these, are always considered.
3) Leverage every encounter with the patient. Think about why a patient is being seen and where. What can be done to ensure that appropriate interventions are considered even when those interventions are unrelated to the reason the patient is being seen. During flu season, for example, almost any interaction with the healthcare system is an opportunity to ensure that the patient receives a flu shot.
4) Think about patients not being seen. Traditionally, healthcare is provided when a patient chooses to be seen. However, population health management requires addressing all patients, not simply the ones who opt to be seen. A strategy needs to be developed to reach out to the patients who aren’t presenting themselves. Ensuring that these patients receive appropriate interventions is critical when trying to meet outcome-based payment goals.
Summary
Value Based Care is a unique opportunity for collaboration across healthcare stakeholders to deliver on the promise of value for patients. The principles of Population Health Management include maximizing Quality through Plan of Care, minimizing Cost via Risk Stratification, and enhancing Experience with Longitudinal Support as key pillars for success.
Voice Biomarkers can provide unique real-time behavioral health signals for risk stratification and triage as well as key longitudinal metadata for advancing patient satisfaction in whole-person care. Technological innovation across Value Based Healthcare models will play a significant role in accelerating VBC adoption as usability from commercial products outside healthcare are brought into the clinical workflow to streamline operations, augment generalists, and personalize care.
We are excited to envision 2030 and beyond where Value Based healthcare will look vastly different from its teenage years, a little more high-tech and a lot more human.
“Any sufficiently advanced technology is indistinguishable from magic.”
- Arthur C. Clarke
Special Thanks
Thank you to the following reviewers for your real world insight, experience, and thought leadership: Joe Mercado, Emma Mason, and Darren Schulte.
Glossary
- Behavioral Health Risk Factors – Behavioral and Mental Health Conditions negatively affected by a person’s overall health.
- Behavioral Risk Factors – Individual behaviors or choices that negatively affect health, such as tobacco use, alcohol use, lack of seatbelt use, dietary choices, etc. Habits that cross that line into Behavioral or Mental Health diagnoses would be included in Behavioral Risk Factors.
- Care Management – Care management is a set of activities intended to improve patient care and reduce the need for medical services by enhancing coordination of care, eliminate duplication, and helping patients and caregivers more effectively manage health conditions. These efforts have demonstrated potential to improve quality and control costs for patients with complex conditions.
- Cohort – A cohort in healthcare is any segment or sub-segment of people based on geography, payer source, employer, disease conditions, specific surgical conditions, etc.
- Cost – Cost, the value equation’s denominator, refers to the total costs of the full cycle of care for the patient’s medical condition, not the cost of individual services. To reduce cost, the best approach is often to spend more on some services to reduce the need for others.
- Health Care Delivery – Involves numerous organizational units, ranging from hospitals to physicians’ practices to units providing single services, but none of these reflect the boundaries within which value is truly created. The proper unit for measuring value should encompass all services or activities that jointly determine success in meeting a set of patient needs. These needs are determined by the patient’s medical condition, defined as an interrelated set of medical circumstances that are best addressed in an integrated way. The definition of a medical condition includes the most common associated conditions — meaning that care for diabetes, for example, must integrate care for conditions such as hypertension, renal disease, retinal disease, and vascular disease and that value should be measured for everything included in that care.
- Health Disparity – A “health disparity” refers to a higher burden of illness, injury, disability, or mortality experienced by one group relative to another. A “health care disparity” typically refers to differences between groups in health insurance coverage, access to and use of care, and quality of care. Health and health care disparities often refer to differences that are not explained by variations in health needs, patient preferences, or treatment recommendations and are closely linked with social, economic, and/or environmental disadvantage. The terms “health inequality” and “inequity” also are used to refer to disparities.
- Health Equity – The Robert Wood Johnson Foundation (RWJF) provides the following definition: “Health equity means that everyone has a fair and just opportunity to be as healthy as possible. This requires removing obstacles to health such as poverty, discrimination, and their consequences, including powerlessness and lack of access to good jobs with fair pay, quality education and housing, safe environments, and health care.”
- Health Literacy – Health Literacy is defined in the Institute of Medicine report, Health Literacy: A Prescription to End Confusion, as “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions.”
- Health literacy requires a complex group of reading, listening, analytical, and decision-making skills, as well as the ability to apply these skills to health situations. For example, it includes the ability to understand instructions on prescription drug bottles, appointment slips, medical education brochures, doctor’s directions and consent forms, and the ability to negotiate complex health care systems.
- Health Outcomes – Health outcomes are changes in health that result from measures or specific health care investments or interventions. Health outcomes include:
- Preventing death after a heart attack through in-hospital care
- Improvements in a patient’s quality of life following surgery for a specific health issue (e.g. improved eye sight following cataract surgery)
- Interdisciplinary Team – A group of health care professionals from diverse fields who work in a coordinated fashion toward a common goal for the patient.
- Risk Stratification – Risk stratification is the process of assigning a risk status to patients and then using this information to direct care. Risk stratification enables providers to identify the right level of care and services for distinct subgroups of patients. At the population level, risk stratification allows care models to be personalized to the needs of patients within each subgroup.
- Social determinants of health (SDoH) – Social determinants of health are the conditions in the environments where people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks.
- Social Risk Factors – Specific adverse social conditions/circumstances that are associated with poor health or health outcomes. Any individual-level SDoH that increases one’s likelihood of poor health can be referred to as a Social Risk factor.
- Value Based Payment (VBP) – Value-Based Payments is a concept by which purchasers of health care (government, employers, and consumers) and payors (public and private) hold the health care delivery system at large (physicians and other providers, hospitals, etc.) accountable for both quality and cost of care.
About Kintsugi
Kintsugi is developing novel voice biomarker software to detect signs of clinical depression and anxiety from short clips of free-form speech, closing mental health care gaps across risk-bearing health systems, saving time and lives. Based in Berkeley, California, Kintsugi is on a mission to provide equitable access to mental healthcare for all.
Join our mailing list for regular updates from Kintsugi